Bay Area hospitals are dealing with what is shaping up to be the third-largest wave of COVID-positive patients yet as local public health officials once again urge residents to take extra precautions to stop the rapidly spreading virus.
The number of COVID-19 patients in Bay Area hospitals reached 940 on Wednesday, just a few beds shy of the August 2021 peak when the delta variant of the virus was surging. We’re still nowhere near the two biggest spikes — 2,028 COVID-19 patients in the pandemic’s first winter in January 2021 and 1,914 last January during the omicron wave.
But this year has its own twist.
“Emergency rooms are packed,” said Dr. Peter Chin-Hong, a UC San Francisco professor of medicine who specializes in infectious diseases.
And it’s not just COVID-19 that is crowding ERs and filling hospital beds. While fewer COVID-19 patients are seriously ill from the virus compared to previous winters, the resurgence of other viruses such as influenza and RSV are combining forces and making it trickier for all of us — and our doctors — to know why we’re feeling so rotten.
“Back in the old days, sure people were sicker, but it was simpler algorithmically” to know it was COVID-19, Chin-Hong said. Now diagnosis and treatment are a more complicated equation, with so many viruses spreading.
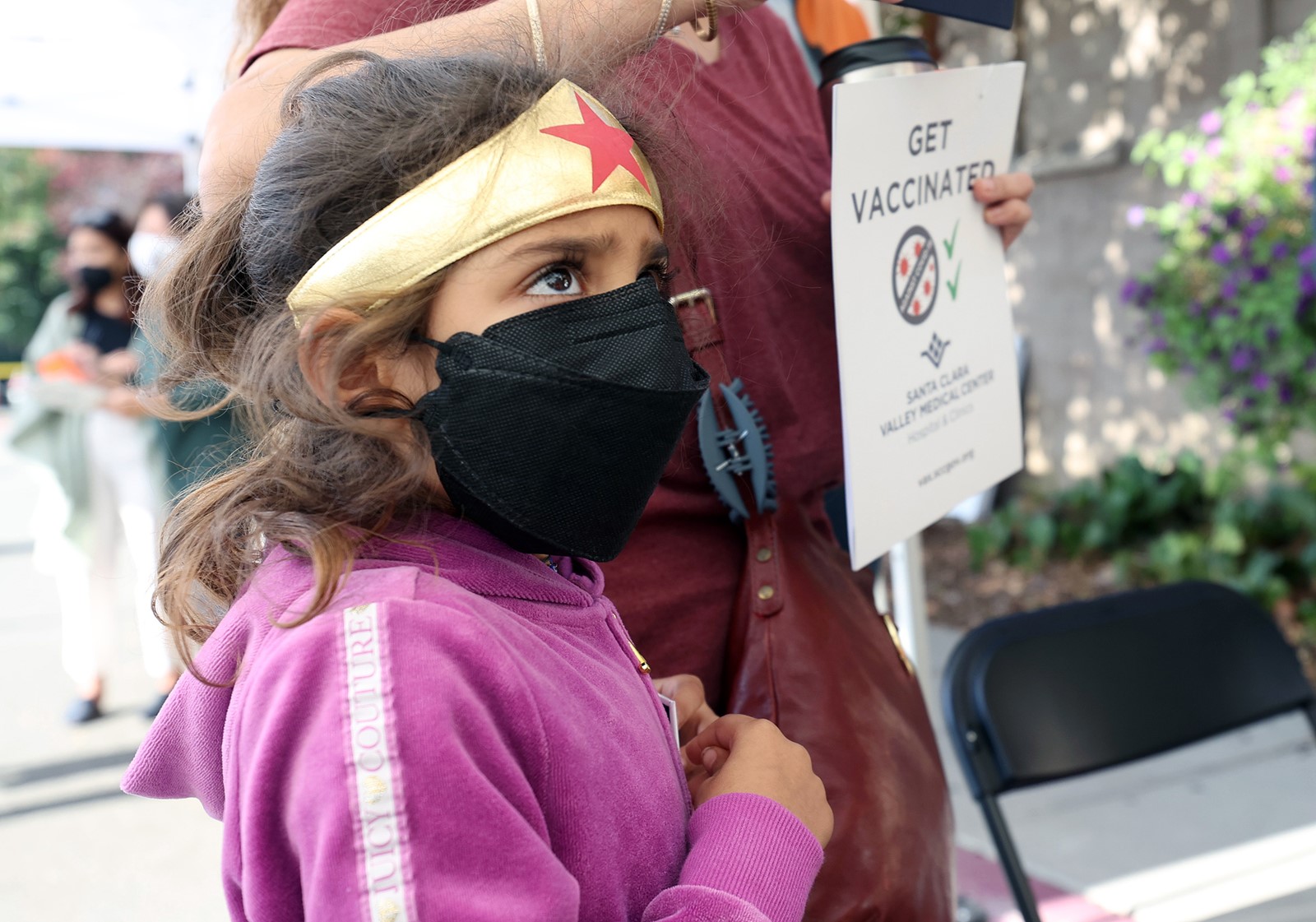
This week, 12 public health directors in the larger Bay Area joined to encourage residents to take precautions and help “ease the burden on local health systems.” They recommend five basic steps: Get vaccinated against flu and COVID-19, stay home if you are sick, wear a mask in indoor public places, get tested if you feel sick, and get treatment if you are.
Limited space isn’t the only challenge health care facilities are struggling with. Chin-Hong said high rates of illness among staff and a current shortage of Tamiflu, used to treat the flu, are contributing to the challenges.
“For every patient that’s admitted to the hospital,” said Dr. Robert Rodriguez, professor of emergency medicine at UCSF and attending physician at Zuckerberg San Francisco General Hospital, “we’re probably seeing another three people who don’t get admitted.” And with emergency rooms having to board admitted patients until space is freed up in the hospital, “that backs us up and inhibits our ability to see patients,” he said.
Karl Sonkin, a spokesperson for Kaiser Permanente, said its facilities in Northern California usually have a daily census of about 3,000 patients. “We are currently seeing an uptick to about 3,500 hospitalized patients,” he said in an email, and 11% of those patients have COVID-19. Like many other facilities, Kaiser has had to increase staffing.
Suzanne Leigh, a spokesperson for UCSF, said the number of COVID-19 patients has doubled to 38 since Nov. 1, but it’s lower than it was on Aug. 1. Just under half of current COVID-positive patients are hospitalized because of their infection, a big difference from early in the pandemic. The rest have what’s considered incidental COVID, meaning they were admitted for other reasons and also tested positive for the virus.
Dr. Niraj Sehgal, chief medical officer for Stanford Healthcare, said over the past week Stanford has 25-35 patients with COVID-19, 10-15 with influenza and 5-10 with RSV. In an email, he said the overall patient numbers “remain exceptionally high.”
For the first two years of the pandemic, the Bay Area’s COVID-19 hospitalization rate was lower than the state’s, but ever since April of this year the tables have turned. For nearly all of the last nine months, the number of patients hospitalized with COVID-19 per 100,000 residents has been higher in the six counties surrounding the San Francisco Bay than in the rest of the state.
While the Bay Area’s COVID-19 hospitalization rate is slightly above the state’s as a whole, other parts of the state are also seeing their hospitals getting slammed. Los Angeles County’s Public Health Director Barbara Ferrer announced on Thursday that hospitals in the county have the lowest number of beds available since before the pandemic, four years ago.
But despite the surge in hospitalizations, there is good news in year three of the pandemic: Thanks to vaccines and therapeutics such as Paxlovid, the severity of COVID-related illnesses is much lower in this wave.
At Stanford, Sehgal said, it has been rare in recent months to see a COVID-19 patient require a ventilator.


 PREVIOUS ARTICLE
PREVIOUS ARTICLE
