Two research groups at the University of Texas at Dallas are exploring a treatment that could improve the recovery of people experiencing post-traumatic stress disorder, or PTSD.
Vagus nerve stimulation, or VNS, used with traditional treatments for PTSD, may help shorten the length of treatment, increase its effectiveness and make the process more tolerable for patients.
The UTD groups are investigating two key research areas. One group is exploring the complex mechanisms that will help scientists understand how and why this treatment works, as the other group runs a clinical trial testing the use of a new device that can deliver the treatment.
For those who experience PTSD, improved recovery can be life-changing, said Robert Rennaker, associate director and distinguished chair at UTD’s Texas Biomedical Device Center.
The vagus nerve (or a set of vagal nerves) makes up the bulk of our body’s parasympathetic nervous system — also known as our “rest and digest” system. Vagal nerves on the left and right sides of our body run from our brain to our large intestine, and they carry a wide range of signals between different organs and systems, including our brain.
They play key roles in functions like digestion, breathing, sensation and memory.
For example, when we are in a high-stress situation, the vagus nerve tells our brain: “This is an important event. Store this memory so you don’t keep putting yourself in the same dangerous situation over and over again,” said Christa McIntyre, an associate professor at UTD and leading researcher in emotional modulation of memory storage.
McIntyre is the principal investigator of a new $2.2 million grant from the National Institute of Mental Health aimed at understanding the mechanisms that make VNS useful in enhancing treatments that help patients with the maladaptive, intrusive and enduring memories that can come from emotionally traumatic experiences.
‘Fear extinction’
When we experience a traumatic or emotional event, said McIntyre, our memory of that event lasts a long time. This means that we may be fearful of any reminders of the threatening event even after it happens. Over time, however, a process called “fear extinction” allows us to create new memories that compete with the old ones.
Although we do not forget what happened, the reminders are no longer fearful once we have developed new associations with them that are not related to the trauma. But that process doesn’t always work perfectly.
“People who have PTSD, unfortunately, show an impairment in their ability to extinguish conditioned fears, and that might be why they develop PTSD in the first place,” said McIntyre.
A standard treatment for PTSD called exposure therapy involves being repeatedly exposed to the reminders of trauma in an effort to extinguish the conditioned fears. But one of the challenges of this therapy is the rate at which patients drop out, since one of the symptoms of PTSD is avoidance of trauma reminders.
This is where VNS may come in. The vagus nerve sends signals to our brain that help enhance our memory of key events. But it also plays a role in pumping the brakes on our fight or flight response, or acting as a “vagal brake.”
Scientists believe that the vagus nerve may be stimulated by adrenaline during stressful situations, making those memories long-lasting.
By electrically stimulating the vagus nerve through VNS, researchers may be able to achieve the same memory-enhancing outcome while bypassing patients’ fight or flight response.
This would mean potentially being able to make the memories that are made in exposure therapy just as strong and long-lasting as the trauma memory, without patients experiencing the physical changes to their bodies that come with fight or flight, said McIntyre. That is the goal of their research.
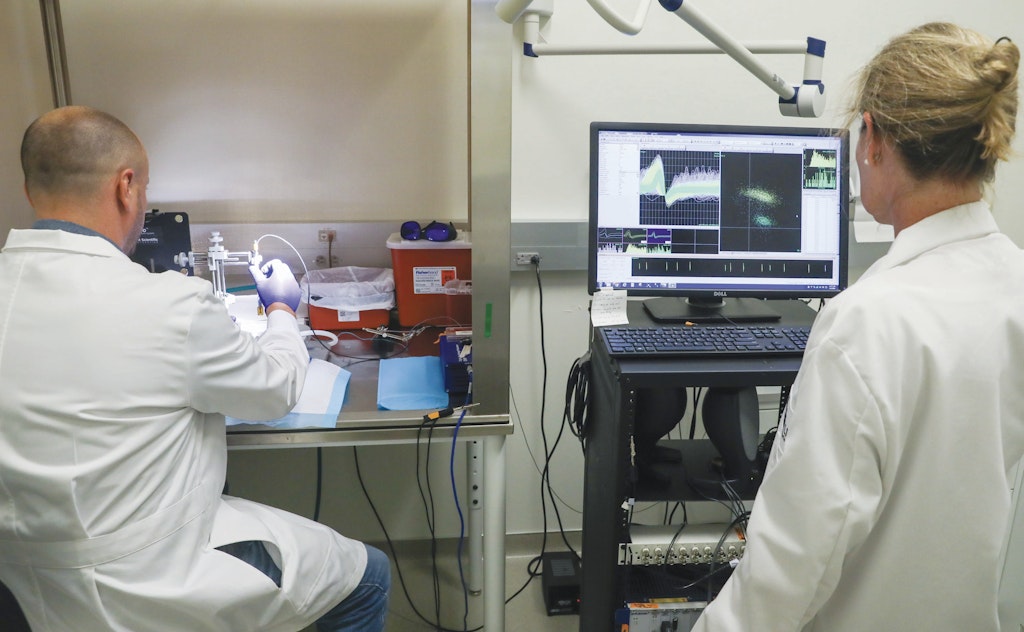
But how does this nerve stimulation actually get administered safely? This is one of the questions Rennaker and his colleagues are working to answer through their trial.
Clinical trial
In any given year, about 12 million adults in the U.S. will experience PTSD. The lifetime occurrence is about 6%. And among veterans, this percentage can more than double, depending on their service era.
Rennaker, who served in the U.S. Marine Corps for five years, is part of a team that is conducting a clinical trial for a small glass device that can be placed on the vagus nerve to electrically stimulate it for several treatments including stroke, spinal cord injury and PTSD recovery. This clinical trial is funded by the Defense Advanced Research Projects Agency, or DARPA.
The device is surgically implanted in participants’ necks during a roughly 30-minute outpatient surgery, and is less invasive than VNS devices that are currently in use for other treatments.
“We designed this solution so that veterans can have all standards of care,” said Rennaker. Because the device is made of glass, patients are still able to receive tests like MRIs and other types of care without any interference with their device.
“They can have whatever they need. And it won’t interfere with the technology, so it never needs to come out,” he said.
Six participants have completed the treatment for PTSD as part of the clinical trial. All have recovered from their PTSD, Rennaker said. Four additional participants will undergo the PTSD treatment with the implanted device and are pending results.
So far, none of the participants have elected to have the device removed — even those who have completed their treatment.
This initial trial is part of three different phases needed to test the device. The next two phases will be “blinded” trials where some participants are stimulated and others are not. This will allow researchers to account for potential placebo effects.
The initial results, however, are promising — particularly considering the success rates of current treatments for PTSD, which are particularly low for veterans.
A class of antidepressants called SSRIs are commonly prescribed for PTSD, said Dr. Imanuel Lerman, a physician scientist at the University of California at San Diego. But only 20% to 30% of civilians experience remission using them. In the veteran population, this efficacy is even lower, said Lerman.
The future of VNS research, scientists hope, will offer patients and those who offer them treatment a way forward. And, as Rennaker emphasizes, the patients are who this is all for.
“I think it’s critical to understand that everything we’re doing is to improve the quality of life for human beings in the U.S. and across the world,” he said.