
When Matt Robert landed in a locked psychiatric unit at Beth Israel Deaconess Medical Center after a suicide attempt in 2006, he said, staff denied his pleas to get some fresh air.
“All I wanted to do was get up, maybe get a little sunlight,’’ he recalled. “I remember saying this, ‘I’ll put leg shackles on. I don’t care. You can tie me to another staff member. Just let me go outside.’’’
Friday, the Massachusetts Department of Mental Health issued new “Fresh Air’’ rules for psychiatric patients across the state. Now the Boston hospital plans to convert a fourth-floor rooftop into a secure patio, giving patients in the 25-bed psychiatric unit an outdoor space, said spokeswoman Jennifer Kritz.
The rules require hospitals to grant mental health patients daily access to the outdoors. But Massachusetts General Hospital and up to a third of psychiatric facilities statewide plan to seek waivers, citing cramped, urban environments.
The rules present a tug-of-war over patients’ rights, doctors’ judgment, and the logistical demands of running a hospital in an urban environment.
Jonathan Dosick, a mental health advocate who has experience being hospitalized for depression and anxiety, came up with the idea over a decade ago after hearing that some patients were not allowed outdoors.
Dosick frames the issue as a fundamental right: “Prison inmates are allowed outside by law,’’ he said. “Even organic livestock, they have laws protecting them. What does that say about people with psychiatric conditions?’’
Robert, who now sits on Beth Israel Deaconess’ Patient Family Advisory Council, agrees.
During his two-week stay, he said, he asked several times to go outside, but staff told him he’d have to wait until he was discharged.
Instead, Robert said, he was confined to the psych unit, which doesn’t have many windows.
“I feel like my stay would have been cut in half if I had had access to fresh air,’’ Robert said.
Other hospitals and psychiatrists, meanwhile, have cited concerns about safety, staffing, space, and liability.
Some private hospitals have also argued that because patients are spending less time in psychiatric beds — an average length of stay of nine days in Massachusetts, instead of months or years — fresh air is not such a crucial concern.
After years of legislative battle, then-Governor Deval Patrick in 2015 signed a law adding “reasonable daily access to the outdoors’’ as a sixth fundamental right for mental health patients. It joined the right to make confidential phone calls, send and receive mail, see visitors, stay in humane living quarters, and communicate with an attorney or advocate.
At least 17 states have similar laws, according to Lauren Roy, an attorney with the Massachusetts-based Mental Health Legal Advisors Committee, which advocates for patients’ rights.
Massachusetts’ “Fresh Air’’ bill took effect April 6, 2015, but didn’t offer practical guidelines on implementation. After a year of wrangling over requirements and exceptions, the state issued regulations Friday.
The new rules include some caveats: Hospitals don’t have to let psychiatric patients outside on demand; they can provide a set time each day. A hospital can also deny outdoor access based on the weather or on the patient’s medical condition, legal status, or risk of running away.
The rules require hospitals to make “reasonable’’ efforts to allow patients outside, including making staffing changes or building an outdoor space. But if a hospital believes it can’t safely do that, it can apply to the state for what amounts to a waiver.
The rules don’t outline any penalty: They simply state that the hospital must demonstrate “to the state’s satisfaction’’ that it is taking reasonable actions given its limitations.
David Matteodo, executive director of the Massachusetts Association of Behavioral Health Systems, which represents 44 of the 59 inpatient psychiatric facilities statewide, said he expects 15 to 20 hospitals to seek exceptions to the outdoor requirements.
Some hospitals, mostly in urban areas, will find it “virtually impossible’’ to comply, Matteodo said. “They just don’t have the capacity to construct a facility outdoors.’’
Mass. General in Boston, which has 24 beds for psychiatric patients, plans to seek an exception based on its location, flanked by high-traffic thoroughfares, with poor access to green space, said Dr. Jeff Huffman, director of the Cardiac Psychiatry Research Program.
Huffman said patients are occasionally escorted out of the unit for a walk around hospital grounds, especially if they are at the hospital for a long time, and the hospital plans to start doing that more often.
Roy, who fought for tougher regulations, said the next step will be for patients to sue or file complaints with the Department of Mental Health if they are denied trips outside.
The Massachusetts Hospital Association supports the law but says it hopes the state provides enough time for hospitals to make necessary changes, said Anuj Goel, vice president for legal and regulatory affairs.
Other hospitals, meanwhile, say they’re already in compliance.
A spokesman for Boston Children’s Hospital, which has 16 psychiatry beds, said kids who stay there can already access a playground, gardens, and other outdoor spaces.
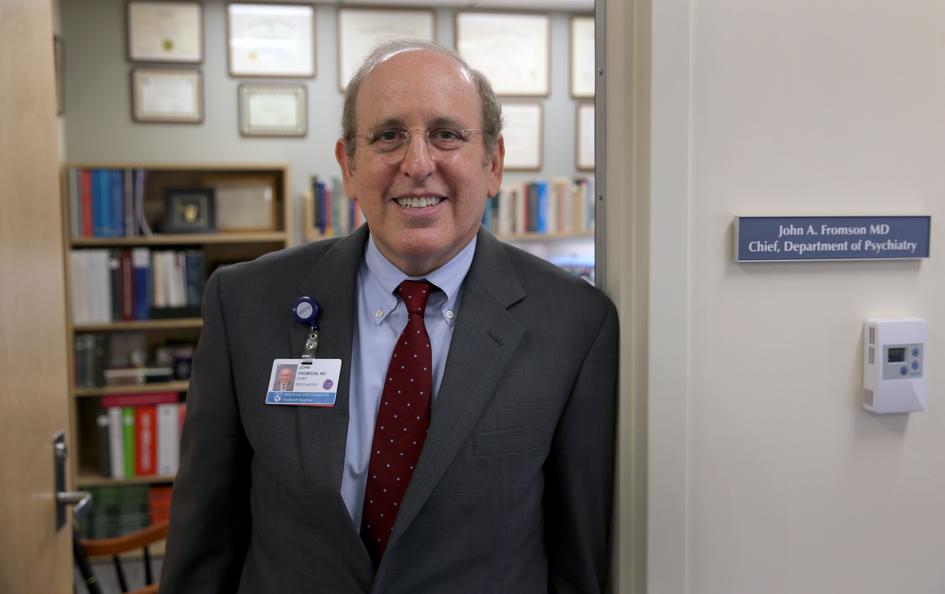
Patients at Brigham and Women’s Hospital who need overnight psychiatric care are sent to the affiliated Faulkner Hospital, which has a 24-bed psychiatric unit for patients 16 years or older, said Dr. John Fromson, chief of psychiatry there.
Patients can walk with a staff escort around the hospital’s grounds in Jamaica Plain — if they aren’t a danger to themselves or others and can follow the lead of the escort, he said.
For the roughly half of the patients who meet that criteria, the walks give them a sense that “there’s life beyond the walls of the hospital,’’ Fromson said. “It’s a nice way to help them transition home.’’
Melissa Bailey can be reached at melissa.bailey@statnews.com. Follow her on Twitter @mmbaily. Follow Stat on Twitter: @statnews.



