The human heart cells had just arrived, and Marianne Kanellias couldn’t wait to take them out of the liquid nitrogen cryostat and insert them into a gelatinous patch that may one day help a person heal after a heart attack.
Kanellias, who graduated from Worcester Polytechnic Institute in May, has spent the past three years volunteering in the laboratory of George Pins, a biomedical engineering professor, on a project to help the heart recover after parts of it die from lack of oxygen.
The team has already knit together a patch of tissue with rat heart cells, and it beats back and forth like pink bubble gum Flubber. Soon, they’ll upgrade to human cells — while also starting the long and arduous process of animal testing required before the Band-Aids stand a chance of helping real people.
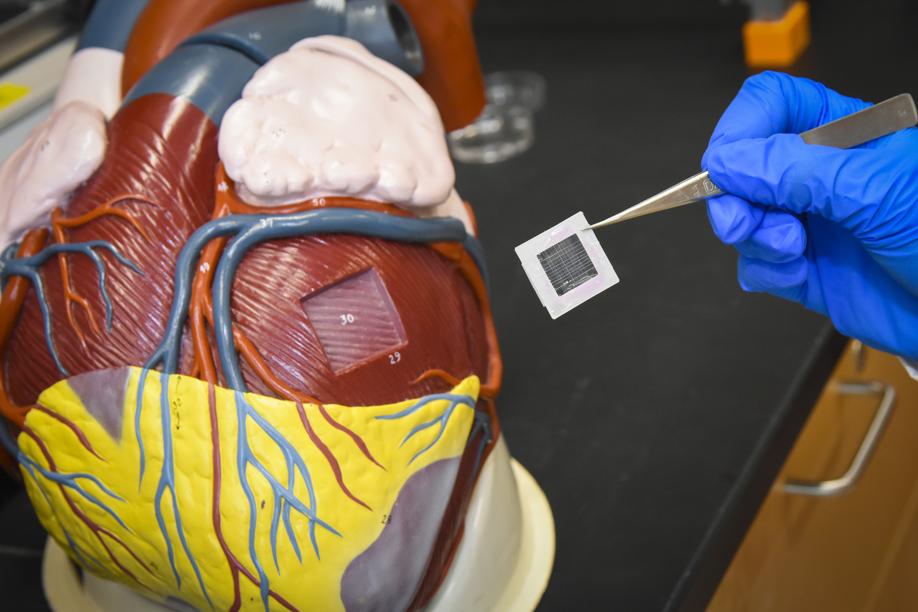
“I want to fix people with heart attacks,’’ Pins said in his office, where a super-size model of the human heart he found in a supply closet 15 years ago sits on his desk. He added, “I think it’s an important global health care problem, and there’s significant unmet need.’’
Millions of people around the world die from heart attacks each year, according to the World Health Organization. And damaged heart tissue doesn’t just heal like a scraped knee — it needs a little help from tissue engineers.
In Worcester, Pins and his students are working on one particular solution: cut out the dead heart tissue and replace it with a personalized patch of hair-thin threads embedded in a goop of custom-grown heart cells.
Scientists around the world have been tackling this problem for decades.
Nenad Bursac, a biomedical engineering professor at Duke University who is part of a recently awarded $8.6 million grant for a similar project, got started over two decades ago in the laboratory of legendary Massachusetts Institute of Technology professor Robert Langer. He said that using threads is one way to make sure the cells line up properly, a necessary feature. Bursac published the first paper to demonstrate how to line up these cells, he said, and to do so, he created a scaffolding on top of real cotton candy.
Kanellias has been building these patches for the past three years as an undergraduate. The process begins simply enough that, when I visited the lab, I was able to try my hand at it with no formal training. But it’s not easy, and my hand-drawn thread turned out thick and gloppy, not thin and uniform.
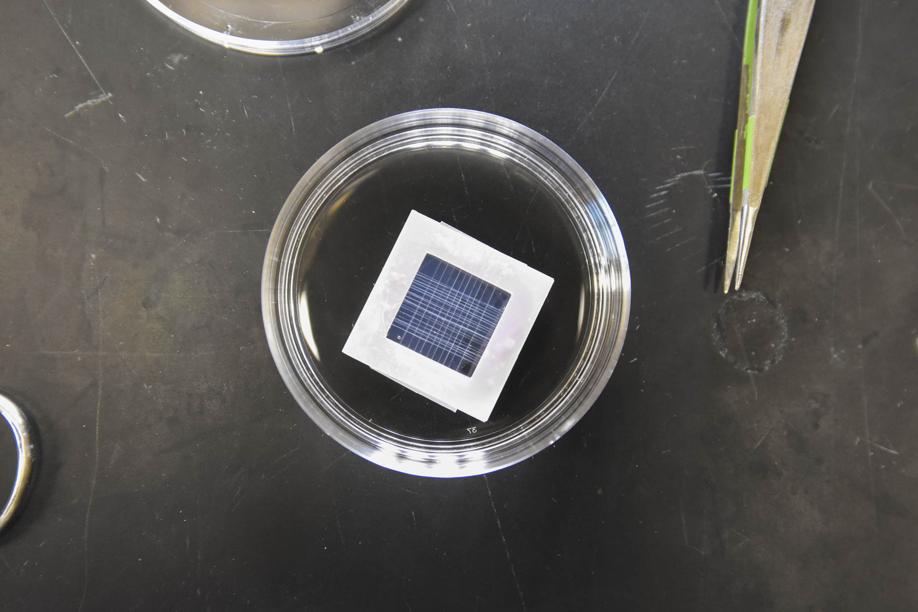
Kanellias has perfected the physical process. First, she paints a line of proteins and enzymes onto a Teflon-coated cookie sheet filled with a chemical solution, and waits for them to combine into a thread. (Mine resembled a bulbous eel, not a sleek cable.) Then she scrapes up the rubbery strand with two pairs of tweezers and sloshes it back and forth in the chemical bath, pulling the thread as it stretches like molten mozzarella.
“This is the wet-stretching technique,’’ Kanellias said. “Basically, stretching it out, and you can see it’s pretty, like — see, I’m trying not to use the word ‘booger-y.’ Do you have a better word for it?’’ she turned to a colleague. “It’s not goopy.’’
“It’s not goopy,’’ concurred Megan Chrobak, a PhD student working on the project. “You could sound science-y and say it’s very elastic.’’
“Elastic,’’ Kanellias agreed definitively.
Then she stretches the thread across a sawed-off cardboard box, pulling until it feels just right, so that it triples in length. (When I tried to stretch a thread, first it snapped, and then got stuck on itself, forming a bauble that looked exactly booger-y.) After it dries overnight, it shines like spider silk, but when handled, it’s brittle and snaps under pressure.
Lined up to form a grid, the threads provide the structure for the patch, which consists of the threads resting in a gel of heart cells and other chemicals. Chrobak said that, in tests of patches made with rat heart cells that will soon be published, the patch behaves similarly to heart tissue from a real live animal.
Nobody in the lab has done rat surgery with these patches — yet. Chrobak said that the first step would be putting one of these patches on top of the heart of a healthy rat to make sure that it’s strong enough to stay in one piece.
Then, they would damage a rat’s heart and put the patch on top of the diseased area to see if it helped the heart function better.
And finally, to see if the patch could work as a replacement for dead heart tissue rather than as a Band-Aid, Chrobak would need to move up to a larger animal — probably a pig, she said.
Bursac’s team has already been doing surgery — and has two papers in the publication process showing how the heart patches work. He’s working together with researchers in Wisconsin, who are making the cells, and scientists in Alabama, who are working on implanting the patches in pigs.
Bursac said that his patches will sit on top of the hearts, and that he won’t be cutting out any tissue.
“Going and cutting out a piece of the heart would likely induce damage in other parts,’’ Bursac said, pointing out that blood vessels run along the surface of the heart. But, he said, “no one really understands what is the best approach.’’
Meanwhile, Kanellias is working on putting human cells, instead of rat cells, into the patches, and testing their response to drugs like epinephrine, which energizes muscle tissue, and 1-heptanol, which calms it down, to see if the patches behave like real human hearts.
STAT
Ike Swetlitz can be reached at ike.swetlitz@statnews.com. Follow him on Twitter @ikeswetlitz.



